All About Male Breast Cancer
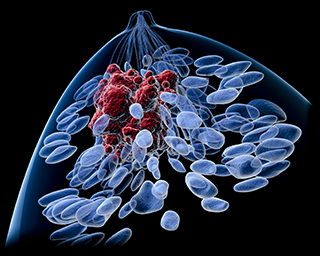
Breast cancer is usually thought of as a female disease, and with good reason: Male breast cancer actually makes up less than 1% of all cases of breast cancer. It is most common in older men, although it can appear in men at any age. Because most men ignore signs of breast cancer, such as a lump, male breast cancer is most often detected at an advanced stage, past the point where it can be treated easily.

Risk factors for male breast cancer include radiation exposure, a family history of breast cancer, a genetic predisposition to breast cancer (e.g., BRCA1 or BRCA2 mutation), and high levels of the hormone estrogen (usually linked to a disease such as liver disease or Klinefelter syndrome).
Symptoms
The most common sign of male breast cancer is a discernable lump in the breast area, usually just below the nipple. Other symptoms may include skin changes near the nipple, discharge from the nipple that is bloody or opaque, or pain in nearby bones (caused by cancer that has spread beyond the breast). Advanced male breast cancer can also cause general feeling of malaise, weakness, and weight loss.
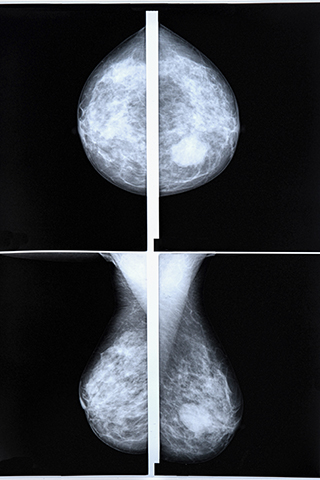
Diagnostic Tests
If your doctor is concerned that you may have male breast cancer, he will order several tests to make a diagnosis. This is usually followed by a clinical breast exam, in which the doctor or professional feels the breast tissue for lumps or other abnormalities. The doctor may then order an ultrasound or an MRI of the breast area in order to see more clearly what the breast tissue looks like and to make an accurate diagnosis.
If the doctor finds a lump, a biopsy may be necessary to determine whether the tissue is cancerous. A biopsy removes some of the tissue, either through using a wide needle or by actually cutting a lump of tissue away from the surrounding area.
Prognosis
If you have received a diagnosis of male breast cancer, your doctor will make decisions about your treatment based on the type of breast cancer, the stage that the cancer has reached, the estrogen-receptor and progesterone-receptor levels in the tissue, your age, and your overall health. In general, the prognosis for male breast cancer is about the same as a female breast cancer prognosis.
Types of Male Breast Cancer
The most common type of male breast cancer diagnosis is infiltrating ductal carcinoma, which originates in the breast ducts and spreads to the surrounding tissue. In contrast, males very rarely get lobular cancers, or cancers that originate in the milk glands, since male breast tissue does not usually contain milk glands. Other common types of male breast cancer include ductal carcinoma in situ (cancer that originates in the milk ducts but has not spread), cystosarcoma phylloides (cancer that originates in the connective tissue around the ducts), and Paget’s disease of the breast (cancer that originates near the nipple).
Keywords: male breast cancer, types of male breast cancer, breast cancer, diagnosis